Nanoscale tent makes diabetes breath test a reality
The accidental creation of a tent mere microns in area has enabled a breath test for diabetes, which could change the lives of millions of people with the disease.
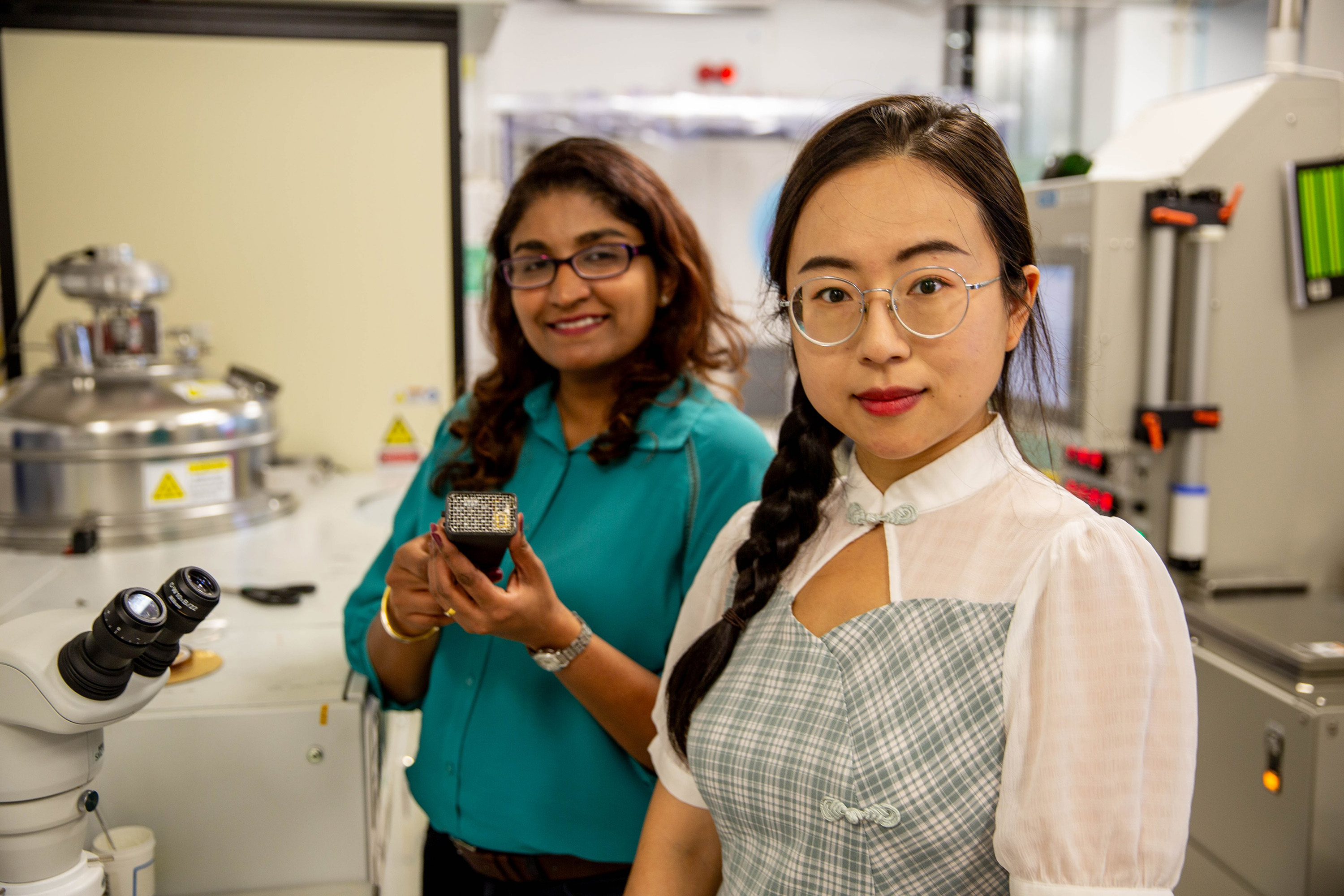
The new device, developed at ANU, could supersede the finger-prick that are a daily burden for people with diabetes, who need to monitor their blood glucose, Dr Buddini Karawdeniya said.
“We’ve had very excited feedback from people living with diabetes, which tells me this is something that will make an impact.”
More than half a billion people suffer from diabetes, and nearly seven million deaths a year are attributable to the disease, in which the body loses the ability to control glucose levels effectively. To monitor their glucose and ketones, people with diabetes need to draw their own blood by pricking their finger.
However, the team from the Department of Electronic Materials Engineering could see a way to remove the need for this regular torment, by harnessing their expertise in nanotechnology gas sensors to create a breath test, part of the ANU research initiative ‘Our Health In Our Hands’ (OHIOH) interdisciplinary project and ARC Centre of Excellence for Transformative Meta-Optical Systems (TMOS).
When the body is low on insulin and cannot use glucose for energy it breaks down fats for energy, creating ketones, such as acetone as a by-product, which can be detected in the breath. So, the team set out to create an acetone sensor based on an ordered semiconductor nanowire array.
As part of her PhD, team member Shiyu Wei had already used this configuration to create a sensor for nitrogen dioxide, a strongly oxidising gas. Acetone has opposite chemical properties: it is weakly reducing, and so the team reasoned that a reduction reaction – contributing electrons – would also give a signal, but of opposite polarity to the oxidative process.
However initial tests were unsuccessful, Ms Wei said.
“We could not detect anything with the original nanowire configuration, which made the investigation very difficult.”
To improve the acetone sensitivity, Ms Wei had to try many different tweaks. Initially she tried doping the indium phosphide nanowires, but found no improvement. Varying the diameter of the nanowires, she found success by halving the diameter to 50 nanometres.
Changing the nanowires’ coating from gold to aluminium was also unsuccessful, but to her relief a platinum coating worked. Subsequent simulations clarified the sensing mechanism was making use of an internal built-in electric field created by the Schottky junction between the platinum and the indium phosphide.
With the sensor now detecting reductive gases, the practical challenge was to make the sensor sensitive to only acetone, and not other possible components of human breath. To solve these kinds of problems the standard approach is to use a coating to functionalise the surface. Dr Karawdeniya drew on her chemistry background, suggesting chitosan, a cheap, biocompatible polysaccharide made from extracts of insects, crustaceans or fungi.
But getting the coating just right also took trial and error. Seeking a high concentration of chitosan, the team along with Dr Krishnan Murugappan from ANU Chemistry tried spin-coating, and electrochemical deposition, but to no avail.
In frustration Ms Wei tried drop-casting – simply putting a droplet of chitosan solution onto the surface and heating it to dry it out – and to her surprise it worked. And she was even more surprised when she put the device under the electron microscope and saw the structure.

Rather than coating the nanowires, as she had expected, the chitosan had formed a layer draped over the top of the nanowires.
“I’d created a structure I’d never seen before, a nanoscale tent! I shared the image with everyone I knew,” Ms Wei said.
The device works via oxygen adsorption onto the chitosan, in the process reducing the oxygen to form negatively charged species. When this interacts with acetone it contributes electrons and creates a pulse of current in the Schottky diode of the nanowire.
The team tried it out with their own breath, spiked with acetone, and were delighted to find that it worked effectively across the whole range of acetone concentrations relevant to diabetes. It also did not detect other common components of human breath such as CO2 or chemicals similar to acetone, such as butanone.
The team worked with the RSPhys electronics workshop to improve an earlier design of a prototype breath test unit, which had been an ANU Engineering Capstone project of OHIOH supervised by Prof Antonio Tricoli and Dr Krishnan Murugappan.
The device, which they named Ketowhistle is reported in Advanced Science.
The prototype went on to win a health technology innovation challenge run by the Australian Centre for Accelerating Diabetes Innovation and shortly undergoing a pilot trial.
The Ketowhistle could be deployed in a number of ways: it may be incorporated into a pregnancy breath test, and also could be used for animal testing: dogs, cats and cows all suffer from diabetes.
Leader of the group Professor Lan Fu is excited to see technology she has worked on set to help patients.
“I think these integrated devices for diagnosis and health monitoring will enable us all to have personalised healthcare, which could transform society in the next 20 to 50 years.”
This article was first published by ANU Research School of Physics.
